Hemoconcentration: Big word, big problem
How hemoconcentration alters test results and how to minimize it
by Dennis Ernst • January 07, 2019
Hemoconcentration. It’s a mouthful. But utter the word in some of your professional circles and you’re likely to win newfound respect for what you know about collecting blood. (See this month’s Tip of the Month below.) But you have to know what you’re talking about. This article will help you understand what hemoconcentration is and how it can affect test results.
If “hemo” means blood, hemoconcentration is an abnormally high concentration of blood. Blood becomes concentrated, or thickens, when the proportion of cells and other larger elements of the blood increases to such a degree that it no longer reflects the patient’s actual health status. Since most of the objective information physicians receive about the well-being of their patients come from laboratory test results, it is critical that specimen collection personnel recognize and prevent situations that lead to hemoconcentration.
During phlebotomy, blood can be concentrated several ways. Patient posture, prolonged tourniquet application, and fist pumping.
Patient posture
The physiology of the blood changes when a patient goes from lying down to upright. Here's why:

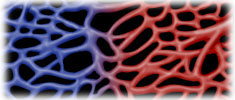
When a person goes from lying down to sitting or standing, the body senses the change in orientation. It knows it’s going to have to do something to keep the brain supplied with blood now that it is "uphill" from the heart. The body---being the marvelous machine it is---responds by releasing hormones into the bloodstream that increase the blood pressure. When blood pressure increases, the brain is continually supplied with oxygenated red blood cells, keeping the patient conscious. However, there's a downside to posture-related changes in blood pressure every phlebotomist must know. The blood circulating throughout the now-upright body becomes instantly hemoconcentrated. That's because when the body senses the circulatory overload from the rise in blood pressure, the capillaries become porous so water and smaller compounds migrate into the tissue. Think of it as a natural "venting" of the circulatory system when it gets the least bit pressurized. What's important for those who draw blood samples to know is that this natural attempt to lower the blood pressure also results in a temporary state of hemoconcentration in the vein you're about to draw blood from.
Think of the sudden porosity of the capillary beds to be like a fishnet, trapping only the larger blood components in the veins. Not only do red blood cells and other cells remain in the circulatory system in a higher concentration temporarily, but so do large substances like proteins and compounds attached to protein that can't pass through the capillary walls because of their molecular size. As a result, they too remain in the bloodstream in temporarily higher concentrations than that in which they existed before the posture change.
Drawing specimens during this change will more than likely lead the laboratory to report a higher test result than if the patient were drawn while recumbent. (1-6) Conversely, when a patient goes from upright to recumbent, the blood is subject to a dilutional effect due to water moving from the tissue into the circulation. It has been reported that cholesterol levels are 10 percent lower and triglycerides 12 percent lower in patients drawn after being recumbent for 5 minutes.(1) Those analytes affected by changes in posture are listed here:(1,7)
- Albumin
- Aldosterone
- Alkaline Phosphatase
- ALT
- Angiotensin
- Antidiuretic hormone
- Bilirubin
- Calcium
- Catecholamines
- Cholesterol
- Drugs
- Renin
- Total Protein
- Triglycerides
Not all of these analytes change to a clinically significant degree. Generally, the change ranges between 5-15 percent.(1) However, all collectors must be aware of the test requirements that specify the patient be recumbent before collection and draw posture-sensitive analytes appropriately. Such requirements are because the effect of hemoconcentration are significant.
Prolonged Tourniquet Application
Hemoconcentration also affects test results when a tourniquet is left on longer than one minute in the same way in which analytes are affected by posture changes. Therefore, when it takes longer than one minute to find and access a vein, hemoconcentration begins affecting test results. That’s why CLSI recommends tourniquets be left on no longer than one minute.(8)
It can be difficult to minimize the time a tourniquet is in place when patients’ veins are difficult to find. Nevertheless, specimen collection personnel shouldn’t rush the vein selection process. Should the survey take more than one minute, CLSI recommends releasing the tourniquet prior to puncture for at least two minutes so that the blood below the tourniquet can equilibrate and hemoconcentration can disperse.
Before releasing the tourniquet, make a mental note of where the vein lies in relation to certain skin “markers” (e.g., freckles, skin creases, contour of the skin, etc.). This can shorten the time it takes to relocate the vein and allow compliance with the one-minute rule.
According to the standards, the tourniquet should be released as soon as the vein is accessed to minimize the effects of hemoconcentration.(8) However, in reality, releasing constriction may interrupt the flow of blood prematurely. Therefore, if the collector feels completing the collection is at risk, he/she should perform the procedure according to what is thought to be best for the patient. It is appropriate to realize not all situations allow for compliance, but knowing the effects of excessive tourniquet time requires the release of the tourniquet upon venous access whenever so doing does not jeopardize the collection.

Fist Pumping
Patients who pump the fist to assist the collector in finding a suitable vein contribute to inaccurate test results. When the muscles are exercised during the constriction of a tourniquet, hemoconcentration results. Studies have been conducted on the effects of fist pumping on potassium and ionized calcium and found them to both be elevated in the arm being used.(1,7-9)
Therefore, collectors should discourage this habit in their patients. Additionally, it is prudent to inform them of the potential for the practice to alter their results. This may serve to prevent them from repeating the behavior in the future.
Google “hemoconcentration” and you’ll come up with about 202,000 hits. Induce it in your patients and your lab is likely to come up with an inaccurate test result. That’s because it is impossible for those who test specimens to know when a specimen is affected by hemoconcentration. When not prevented, it will likely manifest itself as inaccurate results that lead to patient mismanagement. Because physicians rely on laboratory tests heavily to guide their diagnosis, medication and management of the patient, those who draw specimens play a critical role in the proper care of every patient they draw. When hemoconcentration is understood and its causes prevented, specimen collection personnel are more likely to submit specimens to the clinical laboratory that can produce an accurate assessment of the patient’s condition.
References
1. Narayanan S. The preanalytic phase an important component of laboratory testing. Am J Clin Pathol. 2000;113:429-452.
2. Ernst D, Ernst C. Lab Draw Answer Book. Corydon, IN: Center for Phlebotomy Education; 2017.
3. Ernst D. Applied Phlebotomy. Lippincott Williams & Wilkins. Philadelphia, PA. 2005.
4. Becan-McBride K, Garza D. Phlebotomy Handbook. Upper Saddle River, NJ: Pearson; 2014.
5. Sommer S, Warekois R. Phlebotomy Worktext and Procedures Manual. Philadelphia, PA: WB Saunders;2002.
6. McCall R, Tankersley C. Phlebotomy Essentials, Philadelphia, PA: Lippincott Williams & Wilkins; 2015.
7. Dale J. Preanalytic Variables in Laboratory Testing. Lab Med.1998;29:540-545.
8. CLSI. Collection of Diagnostic Venous Blood Specimens. Approved Standard, GP41-A7, Wayne, PA, 2017.9. Baer D, Ernst D, Willeford S, Gambino R. Investigating elevated potassium values. MLO. 2006;38(11):24-31.
Related Posts and Information
overall rating: my rating: log in to rate
error fist hemoconcentration YouTube positioning posture preanalytical preexamination pumping
