Protecting Yourself from Coughing Patients
How to avoid airborne particles from patients who sneeze and cough in your presence
by Dennis Ernst • April 01, 2020
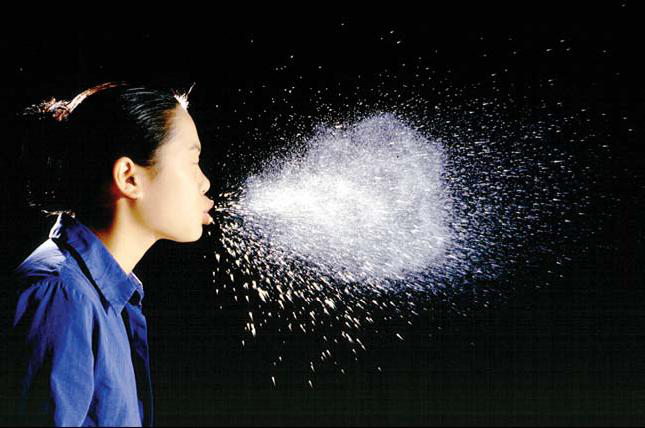
You're bent over with a needle in your patient's arm and he suddenly has a coughing fit, filling the air you breathe with viruses and bacteria. You hold your breath as long as you can to avoid breathing them in, but you can't complete the draw in time. Now it's up to your immune system.
It's flu season. The risk of acquiring any of the myriad respiratory infections that fester within the patient's you'll encounter is real and significant. Influenza-related illness and complications lead to more than 20,000 hospitalizations and 36,000 deaths each year. Some of those patients will come to your drawing area–potentially infecting everyone they come into contact with including you and other patients. A pandemic flu could lead to more than 700,000 hospitalizations and 42 million outpatient visits. This translates into healthcare costs of up to $166 billion.
The Centers for Disease Control and Prevention (CDC) recommends signage at healthcare facility reception areas asking coughing patients to wear a mask or cover their mouth with tissues when they cough. The CDC also requires healthcare facilities to provide a waste can to discard masks and tissues as well as hand sanitizers so that patients may disinfect their hands after each cough. With the threat of pandemic flu growing, taking steps to promote respiratory hygiene is more important than ever. Visually and verbally reminding coughing, sneezing and wheezing patients and visitors of these simple precautions are now a required obligation for healthcare providers, thanks to CDC’s Respiratory Hygiene/Cough Etiquette Guidelines.
A patient continues to hack and wheeze, and can’t seem to consistently cover his cough despite signage and repeated warnings from the receptionist. What should you do to protect yourself? Wear a mask? If so, what kind of mask? Coughing, sneezing patients might only have a common cold; but they could also have a disease as ominous as TB or pandemic flu. So, it is paramount that healthcare professionals who encounter such patients require them to practice respiratory hygiene by either donning a surgical mask or covering their face with a tissue. The healthcare professional should also wear a surgical mask; N-95 masks are only necessary when working in close proximity with TB or pandemic flu patients (the government will issue a pandemic flu warning if it reaches the US).
If not required by your employer, consider getting the flu vaccine annually. Although less than half of health care workers actually get it, the CDC also advises employers to offer free flu vaccine in the workplace to all eligible personnel (including students) during all shifts.
Preventing the spread of respiratory infections requires teamwork between healthcare workers and patients. After you get your flu vaccine this year, remember your role in breaking the chain of respiratory infections: recognize and require coughing patients to wear masks or cover their coughs, and wear a mask yourself when working directly with infected patients.
COVID-19 UPDATE: April 1, 2020

Editor's Note: This article was written long before any of us expected we'd be in the grips of a viral pandemic. While the information above is still relevant today, it's important to provide more current information on this topic in light of the Covid-19 outbreak. The Center for Phlebotomy Education continues to monitor developments and guidance as it pertains to those who draw and handle clinical laboratory samples. We will report what we learn to you in our newsletter and by special bulletins to our newsletter subscribers.
As of 4/1/2020, the CDC has not yet published guidelines specific to phlebotomists and phlebotomy procedures. However, the agency has posted guidelines on its web site for drawing blood from donors. Until more specific guidance is available for diagnostic phlebotomy procedures, the CDC's recommendations to blood donor centers may be applicable, including decontaminating surfaces after ever draw. Keep in mind, routine blood donor screening measures prevent individuals with clinical respiratory infections from donating blood. Those who draw diagnostic blood samples are at far greater risk of acquiring airborne infections.
The best guidance we have found for all healthcare professionals with potential exposure to Covid-19 is the CDC's Interim U.S. Guidance for Risk Assessment and Public Health Management of Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with Coronavirus Disease (COVID-19) published March 7, 2020. It provides guidance for those who have "close contact" with patients potentially infected with Covid-19. (Editor's note: even though the article oddly excludes clinical laboratory personnel as "healthcare personnel," we feel the information contained in it is relevant to those who draw blood samples in the absence of more phlebotomist-specific recommendations.)
The agency defines close contact as:
a) being within approximately 6 feet (2 meters), of a person with COVID-19 for a prolonged period of time (such as caring for or visiting the patient; or sitting within 6 feet of the patient in a healthcare waiting area or room); or
b) having unprotected direct contact with infectious secretions or excretions of the patient (e.g., being coughed on, touching used tissues with a bare hand).
The definition of "prolonged period of time" is hard to define, according to the article, but it suggests "it is reasonable to consider an exposure greater than a few minutes as a prolonged exposure. Brief interactions are less likely to result in transmission; however, clinical symptoms of the patient and type of interaction (e.g., did the patient cough directly into the face of the HCP) remain important."
The article provides guidance on how to react to exposures to known Covid-19 patients. However, to our knowledge the CDC has not issued any recommendations as to which patients constitute a "potential exposure" risk besides those with the obvious symptoms, i.e., fever, cough, and difficulty breathing. However, given the rapid spread of the Coronavirus since this article was published and the virus's asymptomatic incubation phase lasting up to 14 days, every patient should be considered potentially infectious.
For those interested, the CDC hosts a Clinical Laboratory COVID-19 Response Call every Monday at 3:00 PM EDT. Audio and transcripts are posted here. (As of 4/1/2020, this week's call (3/30/20) has not yet been posted.)
Related Posts and Information
overall rating: my rating: log in to rate
airborne biohazardous exposure YouTube infected infection particles sneeze
