Eight Questions Every Phlebotomist MUST Answer Correctly: #7
What do you do when the patient expresses shooting pain?
by Dennis Ernst • June 24, 2021
Question: What do you do when the patient expresses shooting pain?
Anyone who has been drawing blood for even a short period of time has likely encountered a patient who shrieks of pain as the needle is inserted or redirected. What you do when the patient expresses excruciating pain is critical to the safety of the patient and your employer's legal liability should a lasting injury occur. If your reaction to a patient's expression of intense pain is anything less than terminating the attempted venipuncture, you could commit an unforgivable mistake. Read on.
Nerve injury is an inherent risk of phlebotomy. Unfortunately, many healthcare professionals with blood collection responsibilities are not taught the location of the nerves in the antecubital area as part of their training. Were you? To reduce the risk of nerve injury to its lowest degree, become aware of the location of the nerves in the antecubital area. Nerve injuries that occur because the individual lacks an understanding of the anatomy of the antecubital area---or an application of such knowledge---are often indefensible, which translates to liability.
The most frequently injured nerve is the median nerve, which lies in close proximity to the basilic vein and the medial aspect of the median cubital vein. [NOTE: Phlebotomy.com offers a poster depicting the anatomy of the antecubital area, including nerves and precautions when selecting venipuncture sites and veins. An Editorial published in Muscle & Nerve discusses the frequency and severity of nerve injuries during venipunctures. According to the author, nerve injury is far more common than previously suspected, and greater attention should be paid to the proper performance of the procedure. Although data on the frequency of nerve injuries during venipunctures performed for clinical testing does not exist, the editorial states venipunctures performed on volunteer donors for whole blood donation lead to sensory changes including numbness, tingling and burning sensations in approximately one percent of the draws. Out of seven million donations reviewed in 2003, nearly 1600 donors contacted the American Red Cross complaining of post-venipuncture sensory symptoms, while 318 visited a physician for their complaints.
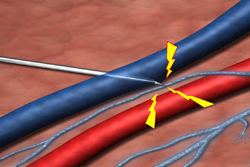
Unlike veins, nerves are neither visible nor palpable and are frequently intertwined with veins. This makes it imperative that specimen collection personnel know the approximate location of the nerves that pass through the antecubital area, and avoid high-risk areas whenever possible. According to the Clinical and Laboratory Standards Institute (CLSI)'s Collection of Diagnostic Blood Specimens, (document GP41), the greatest likelihood of inflicting a nerve injury is in attempting to access a vein on the inside (medial) aspect of the antecubital area. The standard recommends conducting a thorough survey of available veins on both arms for the presence of a median or cephalic vein before selecting the higher-risk basilic vein or the medial aspect of the median cubital vein.
In one study, 90 percent of patients who experienced symptoms of neurological injury were able to trace the onset of their symptoms to needle movement while in the arm. Astute phlebotomists know CLSI forbids lateral (sideways) needle relocation during venipuncture in the medial aspect of the antecubital area where nerves pass in close proximity. Drawing in this area before conducting a search in safer areas (e.g., the center or lateral aspects) doesn't reduce the risk or protect the patient from nerve injury to the greatest extent. Of course, probing in the medial aspect near the basilic vein and brachial artery should never be attempted.
Should the patient express excruciating pain during a venipuncture attempt, the draw must be discontinued and a second attempt made, preferably in a different location. Such expressions of extreme pain indicates nerve involvement, which could lead to permanent injury should the needle remain in the area. Even expressions of tingling or numbness in the hand or fingers should prompt needle removal. To the well-trained and managed phlebotomist (or other healthcare professional with blood-collection responsibilities), tingling or numbness indicates neural activity, which could be caused by the needle's close proximity.
Correct Answer: If a patient expresses excruciating, electric-like, or shooting pain, I loosen the tourniquet and terminate the venipuncture attempt immediately without exception. Even if the patient indicates tingling or numbness in the hand, I remove the needle. I never try to salvage the draw.
Anxious for the rest of the questions? I've compiled all eight into one of our most popular downloads, "Eight Questions Every Phlebotomist Must Answer Correctly."
Related Posts and Information
overall rating: my rating: log in to rate
basilic brachial CLSI median cubital nerve injury YouTube
56 Comments
Thanks Dennis
Great article- very interesting. The 1% statistic is alarming! Your "correct answer" is spot on! Thanks for sharing.
Steve Doerflinger, 06/25/2021 15:09:37
You're welcome
No problem, Steve. Glad you liked it. Thanks for the kind words, my good friend.
Dennis Ernst, 06/25/2021 15:53:18
nerve injury
What I tell my students if they should have a patient experience that appears to have a nerve provocation....Abort mission!!
Terri Mcelhattan, 06/25/2021 16:43:21
Proper Clotting
Is it OK to decrease clot time by allowing tube to clot upside down? Have seen this Don ND want to know if it's correct?
YASHICA L COBBS, 11/15/2021 14:15:46
